Rare 101 – Systemic Amyloidosis
Our commitment to improving the diagnostic odyssey for those affected by rare diseases goes beyond our diagnostic applications, with our disease education blog series we hope to raise awareness and understanding.
The second in our RARE 101 series – Systemic Amyloidosis
What is amyloidosis?
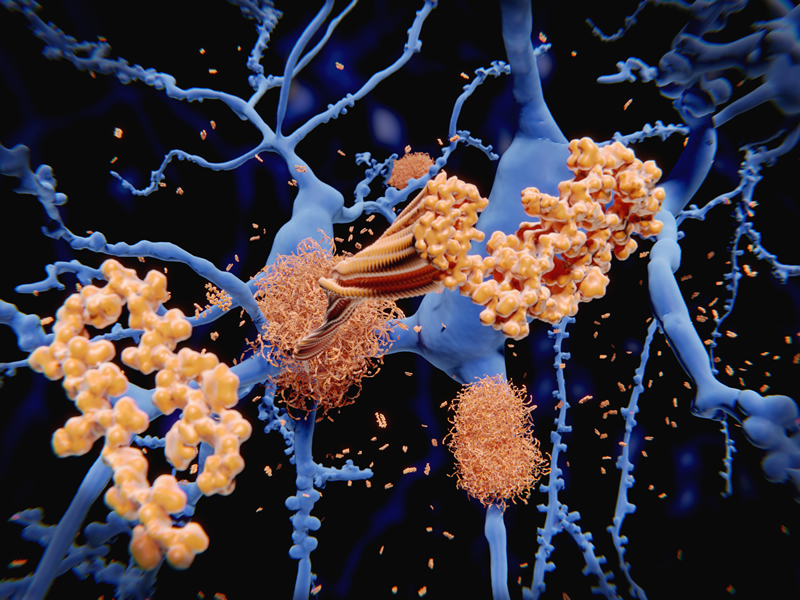
Amyloidosis is a rare disease, caused when certain proteins misfold causing abnormal deposition and accumulation of amyloid fibrils in the tissue, systems and organs of the body. It may be systemic or localised.
What are Amyloid Fibrils?
Amyloid fibrils are protein fibres which are formed when normal soluble body proteins become insoluble, clump together and remain in the tissue instead of being safely flushed away. The aggregated fibrils cause amyloid deposits which accumulate within tissue, systems and organs disrupting their structure and function. There are 30 known proteins that can cause amyloid deposits.
Organs that may be affected by Amyloidosis
Amyloidosis is usually systemic meaning that it may affect many of the bodies organs and systems. Organs that may be affected by systemic amyloidosis include the liver, spleen, kidneys and heart as well as the nervous system, blood vessels, eyes, tongue, skin, the gut and bones and joints.
Amyloidosis Vs. Multiple Myeloma
The complex nature of amyloidosis and the fact that it can mimic other conditions make it very difficult to diagnose. One condition that it is sometimes mistaken for is Multiple Myeloma. Belonging to a group of conditions called Monoclonal Gammopathy, multiple myeloma is a cancerous condition.
Whilst the same cells that cause multiple myeloma can cause amyloidosis, in the case of amyloidosis they no not replicate out of control and invade other areas (as in multiple myeloma) but simply produce the abnormal insoluble protein that forms the amyloid fibrils.
Different types of Amyloidosis
There are several different types of both non-hereditary and hereditary systemic amyloidosis. In this blog we are taking a closer look at Hereditary ATTR. For more information on other types of Amyloidosis please follow the links.
AL amyloidosis
Previously known as primary amyloidosis, AL is currently the most common type of amyloidosis in developed countries. Patients with AL amyloidosis have an underlying disorder which is the cause of an overproduction of amyloidogenic proteins. Left untreated survival rates may be lower than one year.
AA amyloidosis
Previously known as secondary amyloidosis, AA can appear in patients who have experienced chronic inflammatory or infectious diseases over a prolonged period.
AFib amyloidosis
Rare hereditary genetic disease, affecting people with mutations in their gene for fibrinogen. Fibrinogen is a normal blood protein present in us all that is made exclusively by the liver and is essential for blood clotting.
ALys amyloidosis
Hereditary lysozyme amyloidosis was first described by Professor Sir Mark Pepys and colleagues in 1993. A mutation in the lysozyme gene is responsible for the amyloid fibril protein in amyloid deposits.
ATTR amyloidosis (Transthyretin amyloidosis)
In the case of ATTR amyloidosis the amyloid deposits are made from a protein called transthyretin (TTR) and may be hereditary or non-hereditary.
- Non-Hereditary ATTR amyloidosis
Also known as Wild-Type (ATTRwt) affects the elderly (mostly males) and progresses slowly. It is caused when normal ‘wild-type’ TTR proteins misfold and form the amyloid deposits. The main clinical effect of this type of amyloidosis is in the heart, with some cases affecting peripheral neuropathy and causing carpel tunnel syndrome. More on ATTRwt
- Systemic ATTR Amyloidosis (Hereditary)
Hereditary ATTR Amyloidosis is the most commonly recognised form of hereditary amyloidosis. Genetic mutations in the TTR gene cause patients to produce abnormal amyloidogenic TTR throughout their lives. The abnormal TTR protein causes the amyloid deposits to form and build up causing clinical disease mainly in the heart, nerves and in some cases the kidneys, eyes, ligaments and tendons. Over 150 different amyloidogenic variants (mutations) of TTR have been found to date.
Systemic ATTR Amyloidosis (Hereditary) - Signs and Symptoms
Most common symptoms:
- Periphery neuropathy – limb weakness, loss of sensation,
- Autonomic neuropathy – affecting bladder and bowel, sexual dysfunction, blood pressure
- Heart failure – amyloid deposits in the heart cause stiffening of the heart (restrictive cardiomyopathy). Symptoms of this may include: palpitations, breathlessness, weight loss, leg swelling, nausea, fatigue, dizziness & fainting, chest pain, disrupted sleep.
- Other areas disease may occur due to amyloid deposits: Eyes, kidneys, adrenal and thyroid glands and blood vessels.
Onset of symptoms may occur at any age between early 20’s and 80’s however within families the pattern for age, clinical features and progression rate is usually consistent.
Affected Populations?
Hereditary ATTR is found in 1 in 100,000 Caucasians in the U.S with the V122l mutation found in 1 in 25 African Americans. The Val30Met mutation is most widely found in Portugal, Sweden and Japan and the T60A mutation is most common in the UK (usually found in people of Irish ancestry).
It is also thought to be more common but under-diagnosed in regions of Spain, France, Cyprus, Bulgaria, Ireland and Brazil.
How is Hereditary Amyloidosis Disease Diagnosed?
The systemic nature of amyloidosis with a wide spectrum of symptoms that vary from person to person result in amyloidosis being severely under-diagnosed. Doctors may suspect ATTR amyloidosis based on patients’ symptoms, through examination or based on family history. The following tests can be performed to confirm diagnosis.
Tissue Biopsy –a small sample of tissue is taken from the area that is suspected to have amyloid deposits and examined to identify the presence of amyloid fibrils.
Genetic Testing – is used to identify the amyloidogenic mutations in the TTR Gene. With different mutations leading to different types of disease this testing can provide information about the likely clinical direction.
Imaging Test – ECG (echocardiogram) DPD and Cardiac MR scans may be used to detect ATTR amyloid deposits. More can be found about these tests here.
SAP Scan – Invented in 1987 by Sir Mark Pepys the SAP Scan was developed into a harmless and effective routine test which shows amyloid deposits in tissues and organs. Particularly good at showing the extent of the amyloid deposits and used to compare spread and regression. Unfortunately, this is less helpful at detecting ATTR amyloidosis as it cannot detect the amyloid deposits in the heart or nervous systems. DPD testing has proved to be sensitive at detecting deposits in the heart and since 2010 has been used routinely to test patients where heart involvement is suspected.
What Treatments are available for ATTR Amyloidosis?
Treatments currently available to patients differ considerably but are all based on two principles:
- Reducing the amount of proteins that form the amyloid fibrils (precursor proteins).
Liver, heart and combined Liver/Heart transplantations may be used reduce the supply of the amyloid-forming variant TTR, however this option is suitable for only a small number of patients.
- Supporting the function of organs which contain the amyloid deposits.
Diet, fluid balance, pain medications, elastic stockings and medications for blood pressure may all be used to support the affected organs and control symptoms. You can find out more about treatment options here.
New Drugs and Current Studies for ATTR Amyloidosis
There are a number of new drugs in various stages of development which are bringing much hope to the community.
Diflunisal
Diflunisal is a drug belonging to the non-steroidal anti-inflammatory drug category. Diflunisal is bound by TTR in the blood which is presumed to make the TTR less amyloidogenic. Trials are underway to assess the effectiveness on the progression of neuropathy and cardiomyopathy in patients with hereditary ATTR amyloidosis.
Tafamidis
Tafamidis was developed specifically for hereditary ATTR amyloidosis. It is bound by TTR in the blood which is thought to stabilise the TTR making it less amyloidogenic. It was studied in patients with early neuropathy and slightly slower progression was shown in patients who were given the drug and it was approved for use in Europe for polyneuropathy caused by ATTR amyloidosis. However, as the evidence is not strong, it has not been approved by the FDA and is not available on the NHS. However, a new study using tafamidis to treat transthyretin amyloid cardiomyopathy (currently untreatable) has shown promising results. Read more about this study here.
Genetic therapies and treatments
Patisiran
Patisiran belongs to a class of drugs called small interfering RNA (siRNA) drugs. This type of gene therapy is known as ‘gene silencing’. The drug is not intended to repair the faulty TTR gene, rather, ‘silence’ its effects by interfering with TTR production in the liver cells. The Apollo trial is a multi-centre, randomised, double-blind, placebo-controlled, phase 3 trial.
IONIS TTR Rx
IONIS TTR Rx is one of a class of drugs called antisense oligonucleotides which is also a type of gene therapy known as ‘gene silencing’. The purpose of the trial is to determine whether IONIS TTR Rx can slow or stop the nerve damage caused by ATTR deposits in patients with Familial Amyloid Polyneuropathy.
Antibody mediated amyloid elimination
Invented by Sir Mark Pepys, founder of the Centre for Amyloidosis and Acute Phase Proteins and the National Amyloidosis Centre, miridesap was licensed to GlaxoSmithKline in 2009. Designed to remove the normal blood protein serum amyloid P component (SAP) which is also present in amyloid deposits it was hoped that the removal of SAP would allow the body to remove the amyloid deposits of its own accord. The humanised version of the drug dezamizumab is now in clinical trials with very promising early results.
Looking for Support?
The National Amyloidosis Centre (the NAC) is part of the University College London (UCL) and is situated at the Royal Free Hospital in Hampstead, London. The NAC has been at the cutting edge of treatment and research for over 25 years. Since 1999 the NAC has been responsible for the UK national caseload of amyloidosis and is a highly specialised NHS clinical service funded by NHS England.
You can also check the following sites focused on creating support communities around amyloidosis:
References:
http://www.amyloidosis.org.uk/
https://www.nejm.org/doi/full/10.1056/NEJMoa1805689
If you liked this article maybe you will also find interesting the following in-depth articles about other rare diseases, like A Day In The Life Of...Dr Pradeep Ravichandran Speaker Series - GPX4 Gene Mendelian & Modality NHS Partnership